Financial toxicity resulting from huge medical bills
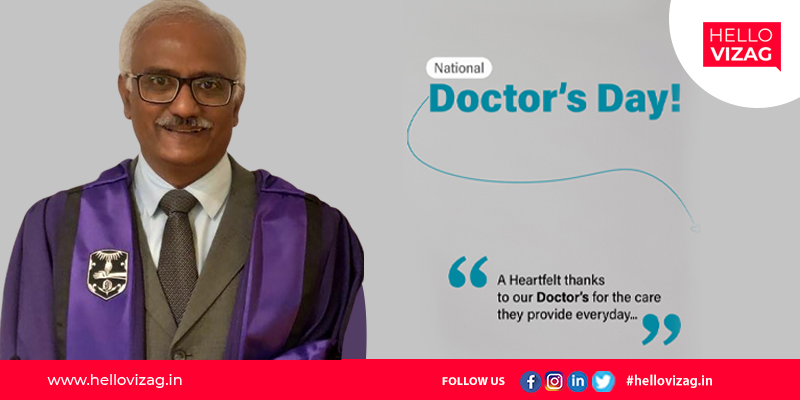
As we celebrate World Doctors Day today, Hello Vizag brings to you how medical treatments and bills can lead to financial toxicity.
During the past few years, medical science has observed rapid advancements, due to which the cost of medical treatment has increased drastically. Medical emergencies or accidents do not happen with prior intimation. It could happen at any point of time and leave us in a state of shock and trauma. Taking care of the patient and ensuring quality medical treatment won’t suffice, arranging sufficient funds for paying the hospital expenses also add on to the tension. To ensure complete peace of mind and fight effectively against illness rather than sourcing finances, prior financial planning is essential.
On the special occasion of Doctor's day, we speak to Dr. D Ragunatharao, Founder Director of Homi Bhabha Cancer Hospital and Research Centre and Chief of Medical Oncology, KIMSs ICON hospital, Visakhapatnam, on how, for instance, cancer may kill one patient but its financial toxicity slays the whole family. Current estimates suggest that out of every 9 Indians, 1 among them will develop cancer in their lifetime. “Despite wide under-reporting of the cancer data, it still gives a glimpse of the huge magnitude of the financial toxicity of cancer treatment.”
But, we were trying to understand better, what exactly is this terminology called financial toxicity? Dr. D Raghunatha Rao clears, “Financial toxicity is a kind of financial distress that a cancer patient and his/her caregivers face due to the direct and indirect cost of the cancer treatment. Though the direct cost of cancer including hospital bills, drugs, lodging, and travel is directly apparent and countable, indirect cost is also substantial and includes days off work, loss of daily wedges, and decreased work efficiency. It is a worldwide problem and is a major cause of bankruptcy. In India also, financial toxicity is a major hurdle in optimum cancer care.”
Over 75% of cancer patients incur out-of-pocket expenses that are not covered by insurance companies or government schemes. The cost of care has become so onerous that some people have ditched going to the doctor altogether. The expert continued, “The financial toxicity is determined by multiple factors. At the patient level, the advanced stage at the presentation is a major issue as over 70-80% of Indian patients still seek treatment very late in the course of the disease. The treatment of advanced-stage usually warrants multi-modality treatment which escalates the treatment cost substantially.
Stating further Mr. Ragunatha Rao said “the cost of so-called 'routine tests' - which are very liable for abuse both by anxious families and enthusiastic doctors can add to the financial toxicity. Many tests included in the so-called "master Health Check up" or executive health check-up are pure JUNK - they are not recommended by any authority to detect any disease whatsoever - yet, they are pushed by corporate hospitals and independent diagnostic labs to gullible customers”. Other patient-related factors are poor insurance coverage, recurrent cancer, education, young age, low household income, geographic location of residence, lack of savings and other social responsibilities.”
“The impacts of financial toxicity are both short-term and long-term for the patients and their caregivers. Immediate fallouts of financial toxicity are poor treatment compliance and, incomplete treatment, and poor quality of life of not only the patients but also the caregivers. It also results in the accumulation of debts for the family. It pushes slowly pushes the family into poverty when they are be deprived of basic life necessities including school dropouts of the children,” Dr. Raghunatha Rao added.
In fact, according to a poll, close to 3 in 10 of the participants said they considered not seeking care to avoid their high deductibles, while more than 20% said they stretched their prescription drugs by taking less than the recommended dosage. With newer treatment options available in the armamentarium of the doctors, the cost of the treatment has also shot up immensely. A six months course of, for example, immunotherapy in recurrent head and neck cancer may cost 12 to 15 lacs to the patients. Other determinants of financial toxicity are low government health expenditure, poorly maintained public hospitals, and poor penetration of care facilities in rural and remote areas forcing the patients to come to metro cities for the treatment.
On buying a health insurance plan, a small fraction of the coverage amount goes as a premium to the insurance company. A policyholder, therefore, expects the insurer to pay the entire hospitalization bill amount to the hospital. However, there could be instances when the insurer pays only a partial amount and the policyholder has to bear the balance as out-of-pocket expenses. In spite of having medical insurance cover, a policyholder may have to pay a portion of the bill to the hospital.
Dr. Rao advises while purchasing a health insurance policy, keep a few important things in mind to make sure there are no out-pocket expenses or they are kept to the minimum. In addition, Dr. Raghunatha Rao says, “Much work needs to be done to alleviate the financial toxicity of cancer care. It requires the broad engagement of patients, doctors, government, public and private hospitals, and NGOs to develop a patient-centered treatment delivery system that integrates effective care with the respective disease economics. Regular awareness and health education programs in the society can encourage the patients to seek care in the early stage of the disease.”
Besides significantly high chances of cure, the cost of the treatment is also substantially low in the early stages as they are usually managed with one treatment modality. The extent of the surgery is limited with minimal postoperative complications and hospital stay in early-stage cancer, bringing down the cost of the treatment significantly. So, health insurance coverage needs to be expanded to contain the out-of-pocket expenditure on care. Other effective measures to reduce financial toxicity are cost transparency, availability of financial counselors, and second treatment opinions.
Dr. Raghunatha Rao says, “The specialists are duty-bound to communicate realistic outcomes to the patients without any prejudice, false hopes or reassurance, and vested interests like new and expensive drugs with marginal survival benefit in days/weeks must not be prescribed as magic drugs. It is the duty of the government to enhance health expenditure for widely available care facilities across the country, including the remote and hilly areas, to ensure successful implementation of Ayushman and other government schemes, to formulate standard treatment guidelines based on evidence-based practice, to bring out the, for example, anticancer drugs price-fixing policy,” he substantiated.
Financial assistance with low-interest rates and staggered repayment options for patients needs to be strengthened through public or private banks. Public-private partnership is an attractive model that needs to be encouraged for consolidating the care facilities in India, especially to bridge the gap in remote areas.